Our Impact - The Brain
Our Impact
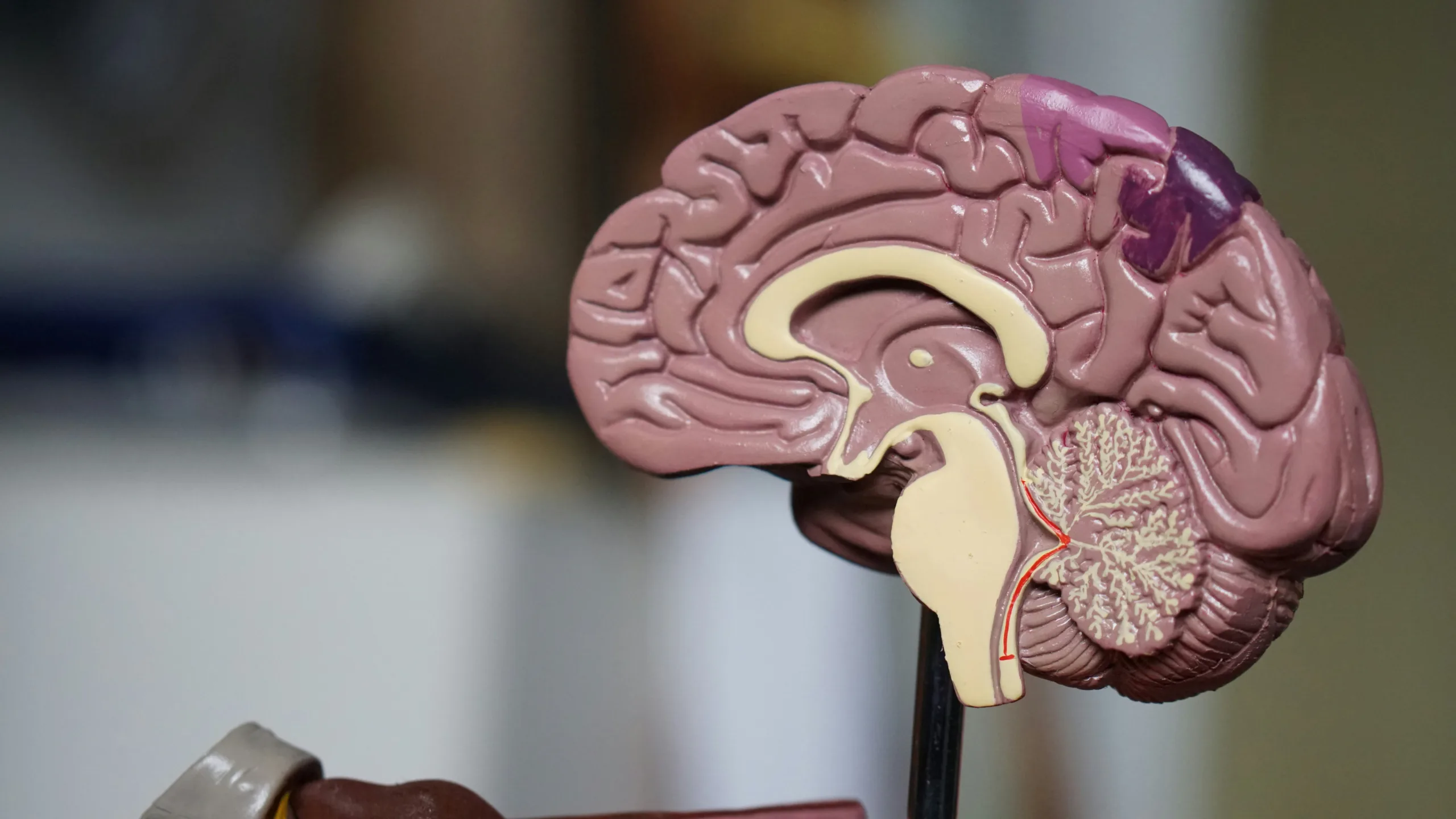
The Brain
Glioma Brain Tumour surgery
Adopting the latest techniques to remove malignant Glioma called fluorescent guided surgery. Fluorescent guided surgery requires the surgery patient to ingest a drug called ‘Gliolan’ which is then selectively absorbed by tumour cells and metabolised into a fluorescent by-product, that can be visualised under a special blue light filter under a microscope. This new technique allows much easier recognition between tumour and normal brain tissue and therefore more complete removal of the tumours which for low grade gliomas is known to improve 5 year survival rates.

Brainlab Navigation System for safer brain and tumour surgery
Thanks to the funding of a new Brainlab Navigation System, POWH was one of the first neurosurgical units in the country to start using stereotaxy which is now considered a standard of care. Stereotaxy is a technique that involves the reproduction of three-dimensional information or an illusion of depth to the sense of touch within an otherwise-flat surface. Stereotaxy systems use cameras to capture and relay the patient’s anatomy and the surgeon’s precise movements in relation to the patient. The surgeon employs tracked surgical instruments in conjunction with preoperative or intraoperative images to indirectly guide the procedure.
Brain cancer research breakthroughs
There are more than 120 different types of brain tumours, which are distinguished by the type of cells they are made of, and their genetic mutations. As tissue is required to make this determination, identifying the specific type of cancer to guide optimal treatment requires surgical sampling. Magnetic Resonance Imaging (MRI) can be used pre-operatively to confirm the presence of a tumour, ascertain its location in the brain, and suggest its likely type. This knowledge is invaluable preoperatively as it can guide how extensive a resection should be, especially when critical parts of the brain are involved. However, MRI resolution differs greatly from the resolution of microscopy, so understanding the microscopic correlates of imaging findings is limited. Through our 2021 Grants Round, Dr Kevin Tay, in collaboration with other specialists at Prince of Wales Hospital and University scientists, were awarded funding to bridge this knowledge gap. The Grant will fund a pilot project to evaluate the translational value of MR microimaging in brain tumour samples. MR microimaging is performed on tissue samples, rather than patients, and can therefore be performed at much higher magnetic field strengths than clinical imaging which allows imaging at a resolution closer to that of microscopy. This technique has previously been applied to prostate cancers, and it is hoped that a better understanding of MRI correlates of tissue microscopy features will eventually lead to more accurate pre-operative diagnosis in brain tumours. Results for journal publications are expected by the end of the research project.




