Our Impact - Cancer
OUR IMPACT
Cancer
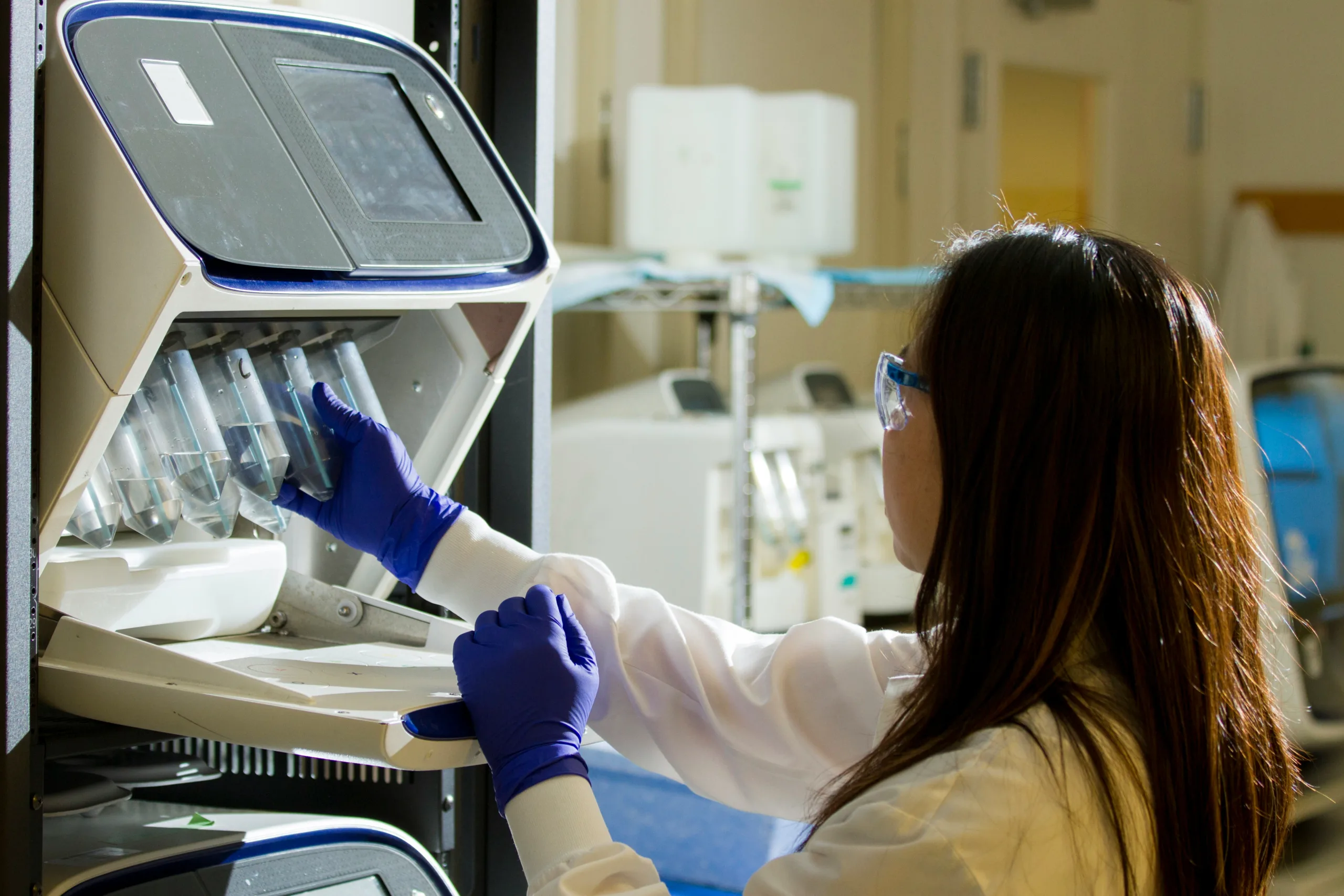
Nelune Comprehensive Cancer Centre
This $79.8 million project is one of the most significant developments in the history of the Randwick Hospitals Campus and we committed over $11M to this vital initiative. The NCCC supports contemporary best practice in the treatment of people with cancer and blood disorders, and brings ambulatory, outpatient and radiotherapy services that were historically provided across eight sites on the Randwick Hospitals Campus into one facility. The NCCC plays a major teaching role in the training of oncologists, radiation therapists, physicists and nurses across the campus and is providing up to 5,000 cancer treatments each year, including patients from regional centres. These state-of-the-art facilities are greatly improving the lives of those living with and recovering from cancer.

Cancer Survivorship Centre
1 in 2 Australians will be diagnosed with cancer in their lifetime and as more people are surviving cancer, the focus has now shifted to holistic and comprehensive post cancer care to ensure the best quality of life after treatment. Cancer survivors are at increased risk for long-term morbidity related to adverse physical and psychosocial consequences of cancer and cancer treatment, but they also deal with the constant worry of recurrence or relapse, the financial burden of cancer treatment as well as fertility concerns. The patient centered evidence-based programs offered at the Prince of Wales Hospital’s Cancer Survivorship Centre are designed to address all these concerns and will help cancer survivors, cancer patients and their families adjust to life after cancer. Supported by us, the Centre opened in 2019 for a short period of time but was then forced to close due to the COVID-19 pandemic. Re-opened in 2022, it was the first and only dedicated Cancer Survivorship Centre in the Sydney Eastern Local Health District.
Head and Neck Cancer Fellowship
We funded a Translational Research and Head & Neck Cancer Fellowship to further expedite care through the Prince of Wales Hospital’s Head & Neck Cancer Rapid Access Clinic. The appointment of Dr Connor O’Meara involves implementation of novel strategies to expedite patient care, exploring integrated reconstruction techniques and researching novel therapies for treatment of Head & Neck Cancers- all aimed to improve treatment access, reduce the impact of disease morbidity and risk of mortality. Dr O’Meara oversees the development of the Head & Neck Cancer Rapid Access Clinic, associated data acquisition and infrastructure streamlining, management and surgical treatment of Head & Neck Cancer patients and the development of a streamlined reconstruction and rehabilitation service for these patients. Since inception, the Head & Neck Cancer Rapid Access Clinic has reviewed more than 12 patients within 3 weeks, completing operations on six patients and reduced the average period of referral to surgical intervention to eight days.
Cancer Survivorship Garden
The funding of the Cancer Survivorship garden means that patients and staff have access to a non-clinical space to enjoy the sun and fresh air, while still being on hospital grounds. The garden is a valued sanctuary and wellness space to rest, recuperate and share time with others. It provides a place of quiet and solitude for those who need to be alone with their thoughts or within the company of others whether that be other patients, staff, family, friends or community members. The design includes lush landscaping with shade trees and native flora, that includes plants with specific health and wellness benefits.
Post cancer fatigue pilot
Fatigue is a common long-term symptom of cancer affecting up to two thirds of survivors, and can persist for months to years after treatment. Fatigue can result in poor quality of life and emotional wellbeing, affecting cancer survivors’ participation in society, vocation and avocational activities. The program will consist of a 16 week group-based program comprising graded physical activity and strength training, in combination with education interventions. The program will be conducted by a qualified exercise physiologist or physiotherapist and a clinical nurse will provide the combined education sessions on nutrition, pain management, mindfulness.





